Utah Leads The Nation (Again) In Mental Illness? What are the accepted reasons and/or rationales behind this?
Utah consistently ranks among the states with the highest prevalence of mental illness, including depression, anxiety, and serious mental illness, as well as some of the highest rates of suicide in the nation. Several accepted reasons and rationales help explain why Utah leads—or is near the top—on these measures:
High Prevalence and Key Statistics
Roughly 22% of adults in Utah report dealing with a mental illness, compared to a national average closer to 19%.
Utah ranks 11th highest for adults with any mental illness, 3rd highest for adults with serious mental illness, and 4th highest for adults with serious thoughts of suicide.
About 40.9% of adults in Utah reported symptoms of anxiety or depression in early 2021, and 26.4% were unable to get needed counseling or therapy.
Suicide is a leading cause of death for Utahns ages 10 to 24.
Accepted Reasons and Rationales
1. Limited Access to Mental Health Care
Utah has a shortage of mental health providers in every county, with fewer providers per 100,000 people than the national average.
Nearly half of Utah’s adults and more than half of Utah’s youth with mental health conditions do not receive the necessary services or treatment.
Cost, lack of insurance, and being forced out-of-network for mental health care are significant barriers.
2. Cultural and Social Pressures
Utah’s strong focus on family, religion, and community can create pressure to conform to social expectations, leading to feelings of isolation for those who feel they don’t fit the traditional mold.
There is a cultural stigma around discussing mental health struggles and seeking help, which can prevent individuals from reaching out and exacerbate feelings of failure or inadequacy.
The “quest for perfection” and reluctance to show weakness are frequently cited as contributing factors.
3. Rural Isolation
Large rural areas in Utah result in many residents being cut off from healthcare services and social support, increasing the risk of untreated mental health conditions.
Rural isolation also makes it harder to access timely and appropriate care.
4. High Rates of Depression and Suicide
Utah has some of the highest rates of depression, especially among teens and young adults.
Suicide rates are among the highest in the country, and suicide is the leading cause of death for young people in the state.
5. Systemic and Structural Issues
Utah’s mental health system is fragmented, with gaps in services and barriers to providing and accessing care.
The COVID-19 pandemic amplified existing pressures on Utah’s limited mental health workforce and increased demand for services.
6. Other Contributing Factors
Substance abuse, traumatic brain injuries, and domestic violence are also cited as factors that increase mental health risks in Utah.
Postpartum depression rates are high, particularly among low-income mothers
What Utah Has Been Doing to Address Mental Illness:
Utah has launched a comprehensive, multi-pronged effort to address its high rates of mental illness and improve behavioral health outcomes. Key actions and strategies include:
1. Major Investments and System Reform
The Utah Legislature has made significant investments in behavioral health services, including ongoing funding for crisis response and intervention programs.
A statewide Behavioral Health Master Plan was developed to guide private and public sectors toward more equitable, aligned, and effective behavioral health systems, emphasizing timely, person-centered, and culturally responsive care.
The Utah Behavioral Health Commission was established to coordinate and assess progress, releasing annual reports and recommendations for system improvements.
2. Crisis Response Expansion
Utah dramatically increased its crisis line workforce and launched the 988 Suicide & Crisis Lifeline, providing 24/7 support for mental health emergencies, suicide prevention, and substance use crises.
The crisis response system has expanded to include mobile crisis outreach teams, community-based behavioral health receiving centers, and plans for new crisis care centers, such as the Kem and Carolyn Gardner Crisis Care Center opening in 2025.
3. Improved Access and Integration
Efforts focus on integrating mental health with primary care, increasing screenings for depression and suicide risk, and improving treatment coordination between providers.
The Huntsman Mental Health Institute has expanded integrated care into dozens of specialty and community clinics, launched collaborative care programs, and placed social workers in primary care settings to streamline behavioral health referrals.
4. Rural and Underserved Community Initiatives
Utah has prioritized improving access in rural areas through grants, telehealth expansion, and specialized training for providers serving rural and underserved populations.
Programs like the Multicultural Rural Mental Health Grant and targeted investments in telehealth have increased services and reduced stigma in hard-to-reach communities.
5. Youth and School-Based Programs
There is a focus on youth mental health, with increased access to school-based mental health services, use of the SafeUT app for crisis support, and programs to ease transitions from inpatient to community care.
6. Ongoing Evaluation and Collaboration
Utah’s approach is iterative, with ongoing evaluation of program impacts, stakeholder engagement, and updates to the Behavioral Health Master Plan based on emerging needs and feedback.
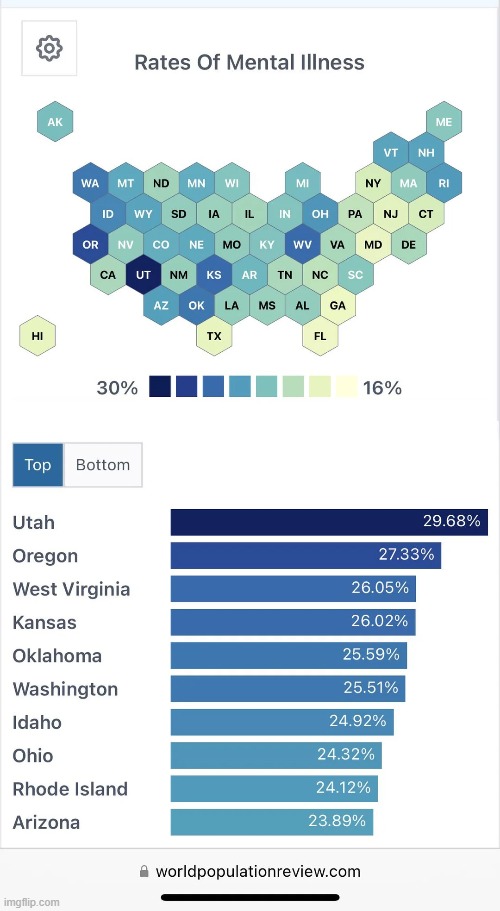
I've heard that the surrounding states around Utah seem to have similar statistics. Is this so? Why?
Yes, Utah's surrounding states—such as Idaho, Wyoming, Nevada, Colorado, New Mexico, Montana, and Arizona—also report high rates of mental illness, suicide, and unmet mental health needs, similar to Utah.
Evidence from Rankings and Data
Utah ranked 51st (last) on adult mental health measures in 2018, with neighboring states like Nevada (50th), Idaho (45th), Montana (34th), and Colorado (40th) also ranking poorly, indicating high prevalence of mental illness and low access to care.
Many of these states share similar challenges, including high suicide rates and shortages of mental health providers, especially in rural areas.
Reasons for Regional Similarities
1. Rural Isolation and Provider Shortages
The Mountain West region is characterized by large rural areas with sparse populations, making access to mental health care difficult. Most counties in Utah and neighboring states are designated as Mental Health Professional Shortage Areas, and the ratio of child psychiatrists is particularly low in Utah, Idaho, and South Dakota.
2. Demographic and Social Factors
The region has a higher proportion of youth and young adults, who are at increased risk for mental health challenges and suicide.
Cultural and social norms in these states can contribute to stigma around mental health, discouraging individuals from seeking help.
3. Economic and Systemic Barriers
Many Mountain West states have lower rates of insurance coverage for mental health and fewer resources devoted to behavioral health services, resulting in higher unmet needs.
4. Shared Environmental and Lifestyle Factors
Factors such as geographic isolation, economic stress in rural communities, and limited social support networks are common across the region and contribute to elevated rates of depression, anxiety, and suicide.
Perplexity A.I.
More information is always better, right Mr. Wang? (think and ponder about Heber C. Kimball and abortion...)